
A more recent article on vitamin B12 deficiency is available.
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2017;96(6):384-389
Author disclosure: No relevant financial affiliations.
Vitamin B12 deficiency is a common cause of megaloblastic anemia, various neuropsychiatric symptoms, and other clinical manifestations. Screening average-risk adults for vitamin B12 deficiency is not recommended. Screening may be warranted in patients with one or more risk factors, such as gastric or small intestine resections, inflammatory bowel disease, use of metformin for more than four months, use of proton pump inhibitors or histamine H2 blockers for more than 12 months, vegans or strict vegetarians, and adults older than 75 years. Initial laboratory assessment should include a complete blood count and serum vitamin B12 level. Measurement of serum methylmalonic acid should be used to confirm deficiency in asymptomatic high-risk patients with low-normal levels of vitamin B12. Oral administration of high-dose vitamin B12 (1 to 2 mg daily) is as effective as intramuscular administration for correcting anemia and neurologic symptoms. Intramuscular therapy leads to more rapid improvement and should be considered in patients with severe deficiency or severe neurologic symptoms. Absorption rates improve with supplementation; therefore, patients older than 50 years and vegans or strict vegetarians should consume foods fortified with vitamin B12 or take vitamin B12 supplements. Patients who have had bariatric surgery should receive 1 mg of oral vitamin B12 per day indefinitely. Use of vitamin B12 in patients with elevated serum homocysteine levels and cardiovascular disease does not reduce the risk of myocardial infarction or stroke, or alter cognitive decline.
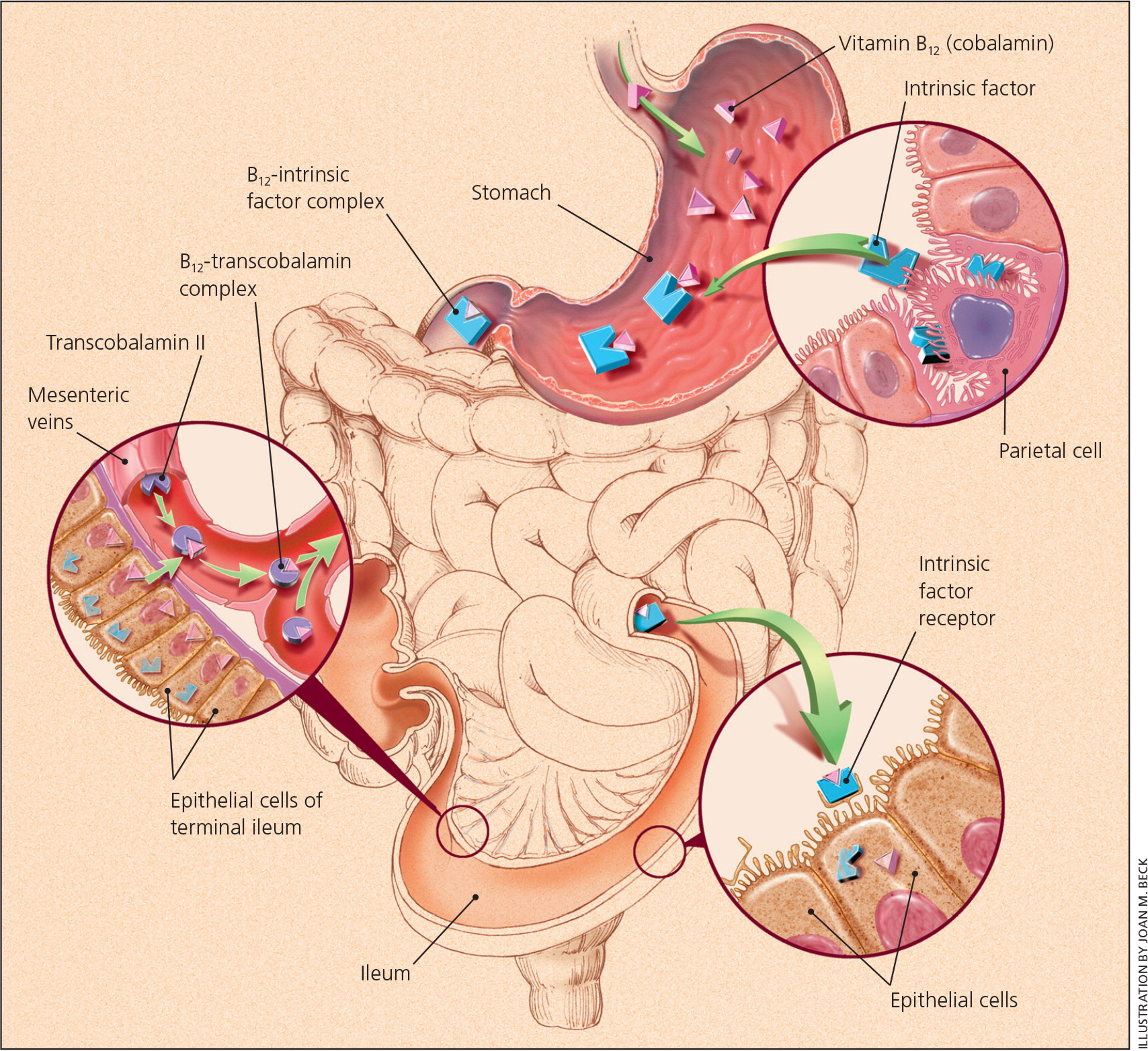
Vitamin B12 (cobalamin) is a water-soluble vitamin obtained through the ingestion of fish, meat, and dairy products, as well as fortified cereals and supplements.1,2 It is coabsorbed with intrinsic factor, a product of the stomach's parietal cells, in the terminal ileum after being extracted by gastric acid1,2 (Figure 13 ). Vitamin B12 is crucial for neurologic function, red blood cell production, and DNA synthesis, and is a cofactor for three major reactions: the conversion of methylmalonic acid to succinyl coenzyme A; the conversion of homocysteine to methionine; and the conversion of 5-methyltetrahydrofolate to tetrahydrofolate.1,2
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Patients with risk factors for vitamin B12 deficiency should be screened with a complete blood count and serum vitamin B12 level. | C | 18 |
| A serum methylmalonic acid level may be used to confirm vitamin B12 deficiency when it is suspected but the serum vitamin B12 level is normal or low-normal. | C | 18 |
| Oral and injectable vitamin B12 are effective means of replacement, but injectable therapy leads to more rapid improvement and should be considered in patients with severe deficiency or severe neurologic symptoms. | B | 18 |
| Patients who have had bariatric surgery should receive 1 mg of oral vitamin B12 per day indefinitely. | C | 31 |
In the United States and the United Kingdom, the prevalence of vitamin B12 deficiency is approximately 6% in persons younger than 60 years, and nearly 20% in those older than 60 years.1 Latin American countries have a clinical or subclinical deficiency rate of approximately 40%.1 The prevalence is 70% in Kenyan school children, 80% in East Indian preschool-aged children, and 70% in East Indian adults.1 Certain risk factors increase the prevalence of vitamin B12 deficiency (Table 1).4,5 Dietary insufficiency, pernicious anemia (i.e., an autoimmune process that reduces available intrinsic factor and subsequent absorption of vitamin B121,2,6,7), and long-term use of metformin or acid-suppressing medications have been implicated in B12 deficiency.8,9
| Decreased ileal absorption |
| Crohn disease |
| Ileal resection |
| Tapeworm infection |
| Decreased intrinsic factor |
| Atrophic gastritis |
| Pernicious anemia |
| Postgastrectomy syndrome (includes Roux-en-Y gastric bypass) |
| Genetic |
| Transcobalamin II deficiency |
| Inadequate intake |
| Alcohol abuse |
| Patients older than 75 years |
| Vegans or strict vegetarians (including exclusively breastfed infants of vegetarian/vegan mothers) |
| Prolonged medication use |
| Histamine H2 blocker use for more than 12 months |
| Metformin use for more than four months |
| Proton pump inhibitor use for more than 12 months |
A multicenter randomized controlled trial of 390 patients with diabetes mellitus showed that those taking 850 mg of metformin three times per day had an increased risk of vitamin B12 deficiency (number needed to harm = 14 per 4.3 years) and low vitamin B12 levels (number needed to harm = 9 per 4.3 years) vs. placebo.8 This effect increased with duration of therapy, and patients had an unclear prophylactic supplementation response. 8 A case-control study that compared 25,956 patients who had vitamin B12 deficiency with 184,199 control patients found a significantly increased risk of vitamin B12 deficiency in patients who had taken proton pump inhibitors (odds ratio = 1.65) or histamine H2 blockers (odds ratio = 1.25) for at least two years.9 In light of these findings, long-term use of these medications should be periodically reassessed, particularly in patients with other risk factors for vitamin B12 deficiency.8,9
Manifestations
Vitamin B12 deficiency affects multiple systems, and sequelae vary in severity from mild fatigue to severe neurologic impairment 1,2,6,10 (Table 24,10). The substantial hepatic storage of vitamin B12 can delay clinical manifestations for up to 10 years after the onset of deficiency.11 Bone marrow suppression is common and potentially affects all cell lines, with megaloblastic anemia being most common.1,2,6 The resultant abnormal erythropoiesis can trigger other notable abnormal laboratory findings, such as decreased haptoglobin levels, high lactate dehydrogenase levels, and elevated reticulocyte count.1,2,6 Symptoms typically include being easily fatigued with exertion, palpitations, and skin pallor.1,2,6 Skin hyperpigmentation, glossitis, and infertility have also been reported.1,2,6 Neurologic manifestations are caused by progressive demyelination and can include peripheral neuropathy, areflexia, and the loss of proprioception and vibratory sense. Areflexia can be permanent if neuronal death occurs in the posterior and lateral spinal cord tracts.1,2,6,12 Dementia-like disease, including episodes of psychosis, is thought to be associated with more severe and chronic deficiency, although supporting evidence is poor.1,12 [corrected] Clinical evaluation seems to show an inverse relationship between the severity of megaloblastic anemia and the degree of neurologic impairment.2
| Cutaneous |
| Hyperpigmentation |
| Jaundice |
| Vitiligo |
| Gastrointestinal |
| Glossitis |
| Hematologic |
| Anemia (macrocytic, megaloblastic) |
| Leukopenia |
| Pancytopenia |
| Thrombocytopenia |
| Thrombocytosis |
| Neuropsychiatric |
| Areflexia |
| Gait abnormalities |
| Irritability |
| Loss of proprioception and vibratory sense |
| Olfactory impairment |
| Peripheral neuropathy |
Maternal vitamin B12 deficiency during pregnancy or while breastfeeding may lead to neural tube defects, developmental delay, failure to thrive, hypotonia, ataxia, and anemia.4,13–16 Women at high risk or with known deficiency should supplement with vitamin B12 during pregnancy or while breastfeeding.4,14–16
Screening and Diagnosis
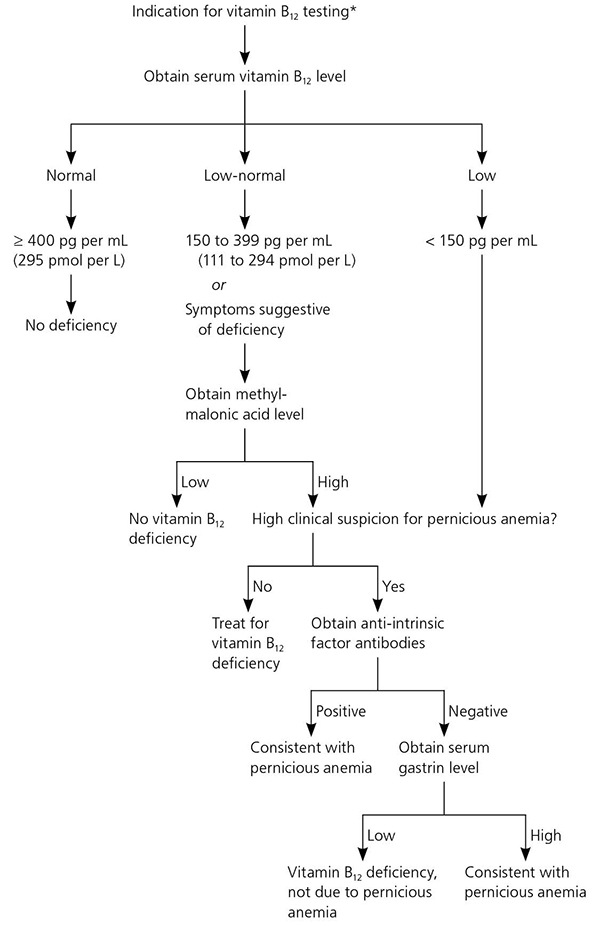
The recommended laboratory evaluation for patients with suspected vitamin B12 deficiency includes a complete blood count and serum vitamin B12 level.2,19–21 A level of less than 150 pg per mL (111 pmol per L) is diagnostic for deficiency.1,2 Serum vitamin B12 levels may be artificially elevated in patients with alcoholism, liver disease, or cancer because of decreased hepatic clearance of transport proteins and resultant higher circulating levels of vitamin B12; physicians should use caution when interpreting laboratory results in these patients.22,23 In patients with a normal or low-normal serum vitamin B12 level, complete blood count results demonstrating macrocytosis, or suspected clinical manifestations, a serum methylmalonic acid level is an appropriate next step 1,2,6,18 and is a more direct measure of vitamin B12's physiologic activity.1,2 Although not clinically validated or available for widespread use, measurement of holotranscobalamin, the metabolically active form of vitamin B12, is an emerging method of detecting deficiency.1,2,18 Table 3 lists the relative sensitivities and specificities of various laboratory tests.24
| Criteria | Sensitivity (%) | Specificity |
|---|---|---|
| Decreased serum vitamin B12 level (< 200 pg per mL [148 pmol per L]) | 95 to 97 | Uncertain |
| Elevated serum methylmalonic acid level | > 95 | Uncertain |
Pernicious anemia refers to one of the hematologic manifestations of chronic auto-immune gastritis, in which the immune system targets the parietal cells of the stomach or intrinsic factor itself, leading to decreased absorption of vitamin B12.1 Asymptomatic autoimmune gastritis likely precedes gastric atrophy by 10 to 20 years, followed by the onset of iron-deficiency anemia that occurs as early as 20 years before vitamin B12 deficiency pernicious anemia.25
Patients diagnosed with vitamin B12 deficiency whose history and physical examination do not suggest an obvious dietary or malabsorptive etiology should be tested for pernicious anemia with anti-intrinsic factor antibodies (positive predictive value = 95%), particularly if other autoimmune disorders are present.1,2,6,18 Patients with pernicious anemia may have hematologic findings consistent w ith normocytic anemia.1 If anti-intrinsic factor results are negative but suspicion for pernicious anemia remains, an elevated serum gastrin level is consistent with the diagnosis.2 The Schilling test, which was once the diagnostic standard for pernicious anemia, is no longer available in the United States. Figure 2 presents an approach to diagnosing vitamin B12 deficiency and pernicious anemia.18,26
Treatment
Vitamin B12 deficiency can be treated with intramuscular injections of cyanocobalamin or oral vitamin B12 therapy. Approximately 10% of the standard injectable dose of 1 mg is absorbed, which allows for rapid replacement in patients with severe deficiency or severe neurologic sy mptoms.2 Guidelines from the British Society for Haematology recommend injections three times per week for two weeks in patients without neurologic deficits.18 If neurologic deficits are present, injections should be given every other day for up to three weeks or until no further improvement is noted. Table 4 lists the usual times until improvement for abnormalities associated with vitamin B12 deficiency.27 In general, patients with an irreversible cause should be treated indefinitely, whereas those with a reversible cause should be treated until the deficiency is corrected and symptoms resolve.1 If vitamin B12 deficiency coexists with folate deficiency, vitamin B12 should be replaced first to prevent subacute combined degeneration of the spinal cord.1 The British Society for Haematology does not recommend retesting vitamin B12 levels after treatment has been initiated, and no guidelines address the optimal interval for screening high-risk patients.18
| Abnormality | Expected time until improvement |
|---|---|
| Homocysteine or methylmalonic acid level, or reticulocyte count | One week |
| Neurologic symptoms | Six weeks to three months |
| Anemia, leukopenia, mean corpuscular volume, or thrombocytopenia | Eight weeks |
A 2005 Cochrane review involving 108 patients with vitamin B12 deficiency found that high-dose oral replacement (1 mg to 2 mg per day) was as effective as parenteral administration for correcting anemia and neurologic symptoms.28 However, oral therapy does not improve serum methylmalonic acid levels as well as intramuscular therapy, although the clinical relevance is unclear.29 There is also a lack of data on the long-term benefit of oral therapy when patients do not take daily doses.2 There is insufficient data to recommend other formulations of vitamin B12 replacement (e.g., nasal, sublingual, subcutaneous).2 The British Society for Haematology recommends intramuscular vitamin B12 for severe deficiency and malabsorption syndromes, whereas oral replacement may be considered for patients with asymptomatic, mild disease with no absorption or compliance concerns.18
Prevention
Because of potential interactions from prolonged medication use, physicians should consider screening patients for vitamin B12 deficiency if they have been taking proton pump inhibitors or H2 blockers for more than 12 months, or metformin for more than four months.5 The average intake of vitamin B12 in the United States is 3.4 mcg per day, and the recommended dietary allowance is 2.4 mcg per day for adult men and nonpregnant women, and 2.6 mcg per day for pregnant women.30 Patients older than 50 years may not be able to adequately absorb dietary vitamin B12 and should consume food fortified with vitamin B12.30 Vegans and strict vegetarians should be counseled to consume fortified cereals or supplements to prevent deficiency. The American Society for Metabolic and Bariatric Surgery recommends that patients who have had bariatric surgery take 1 mg of oral vitamin B12 per day indefinitely.31
Vitamin B12 and Hyperhomocysteinemia
Vitamin B12 deficiency is a much more common cause of hyperhomocysteinemia in developed countries than folate deficiency because of widespread fortification of food with folate. Although epidemiologic studies have shown an association between vascular disease and hyperhomocysteinemia, large randomized controlled trials have shown that lowering homocysteine levels in these patients does not reduce the number of myocardial infarctions or strokes, or improve mortality rates.32 Similarly, an association between elevated homocysteine levels and cognitive impairment has been noted, but subsequent vitamin B12 replacement does not have preventive or therapeutic benefit.33
This article updates previous articles on this topic by Langan and Zawistoski,4 and by Oh and Brown.3
Data Sources: A PubMed search was completed in Clinical Queries using the key terms vitamin B12, cobalamin, deficiency, and treatment. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Also searched were the Agency for Healthcare Research and Quality evidence reports, Clinical Evidence, the Cochrane database, Essential Evidence, the Institute for Clinical Systems Improvement, the National Guideline Clearinghouse database, and the U.S. Preventive Services Task Force. Search dates: March 1, 2016; October 20, 2016; and June 9, 2017.
